Midwives do assisted insemination
This article is presented in 2 formats for accessibility reasons.
The zine format is presented first.
The text-only format is presented second.
*All links referenced in this article can be accessed by clicking the buttons below to learn more.
Midwives Do Assisted Insemination
Written by Rae P. Jimenez, MSM LM CPM
There’s a common misconception (no pun intended) among the TTC (“trying to conceive”) community that assisted insemination services or procedures can only be done in a medical industrial complex such as an infertility clinic.
And while higher-intervention procedures such as IVF (in vitro fertilization), egg retrieval, or infertility diagnostic testing are currently limited to physician-run clinics, other professionals are also able to offer low-intervention fertility services in smaller, private clinics.
Midwives, nurse-practitioners, naturopaths, and a handful of other medical professionals may choose to expand their clinical competency to include a number of preconception services such as nutrition, hormonal support, herbal medicine, or assisted insemination services.
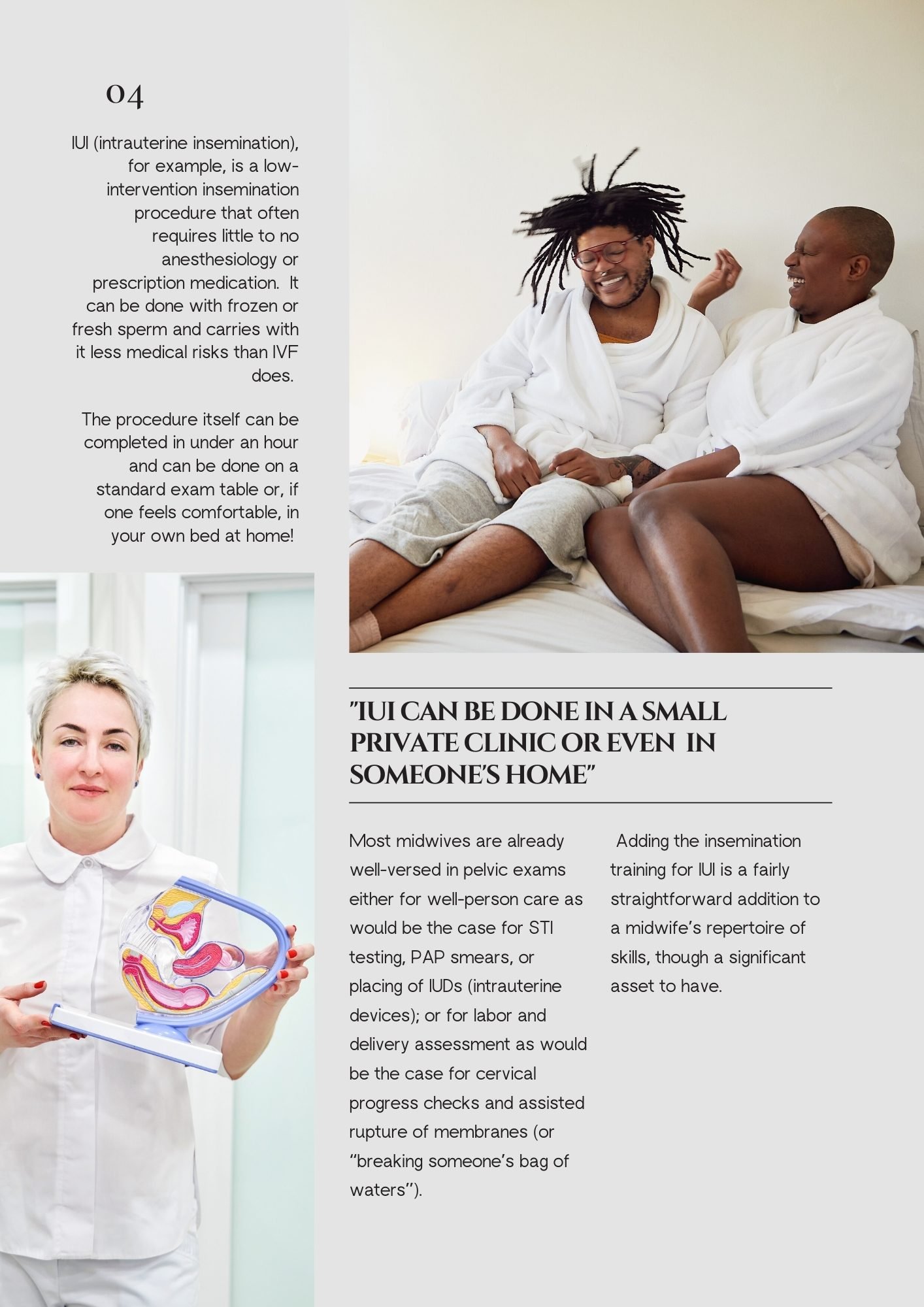
IUI (intrauterine insemination), for example, is a low-intervention insemination procedure that often requires little to no anesthesiology or prescription medication. It can be done with frozen or fresh sperm and carries with it less medical risks than IVF does.
The procedure itself can be completed in under an hour and can be done on a standard exam table or, if one feels comfortable, in your own bed at home!
For this reason, there is a growing number of midwives offering at-home IUI and other fertility services.
Most midwives are already well-versed in pelvic exams either for well-person care as would be the case for STI testing, PAP smears, or placing of IUDs (intrauterine devices); or for labor and delivery assessment as would be the case for cervical progress checks and assisted rupture of membranes (or “breaking someone’s bag of waters”). Adding the insemination training for IUI is a fairly straightforward addition to a midwife’s repertoire of skills, though a significant asset to have.
In the LGBTQ+ community especially, having access to an inclusive and safe provider who also offers fertility services can be a transformational experience in someone’s family-building journey. Queer and trans folx are at higher risk of experiencing common challenges in large medical complexes such as:
· Being continuously misgendered
· Anatomy & body parts being referred to in binaries that are not affirming
· Misconceptions about who is the “parent” vs “gamete donor” vs “gestational carrier”
· Body or identity dysphoria when in a space that does not center or display the diversity of queer and trans families
· Judgements about one’s capabilities to make a baby, especially for those choosing solo conception or polyamory family structures
Midwives choosing to offer fertility services are more likely to have spent additional competency training or even themselves identify with the queer and trans community; intentionally tailoring their care to be more personalized, centering, and informed.
In the same way that many families choose midwives for the increased time, attention, and shared-decision making model of prenatal, postpartum, and birth care, the LGBTQ+ community is increasingly choosing midwifery care as the model for their fertility needs as well.
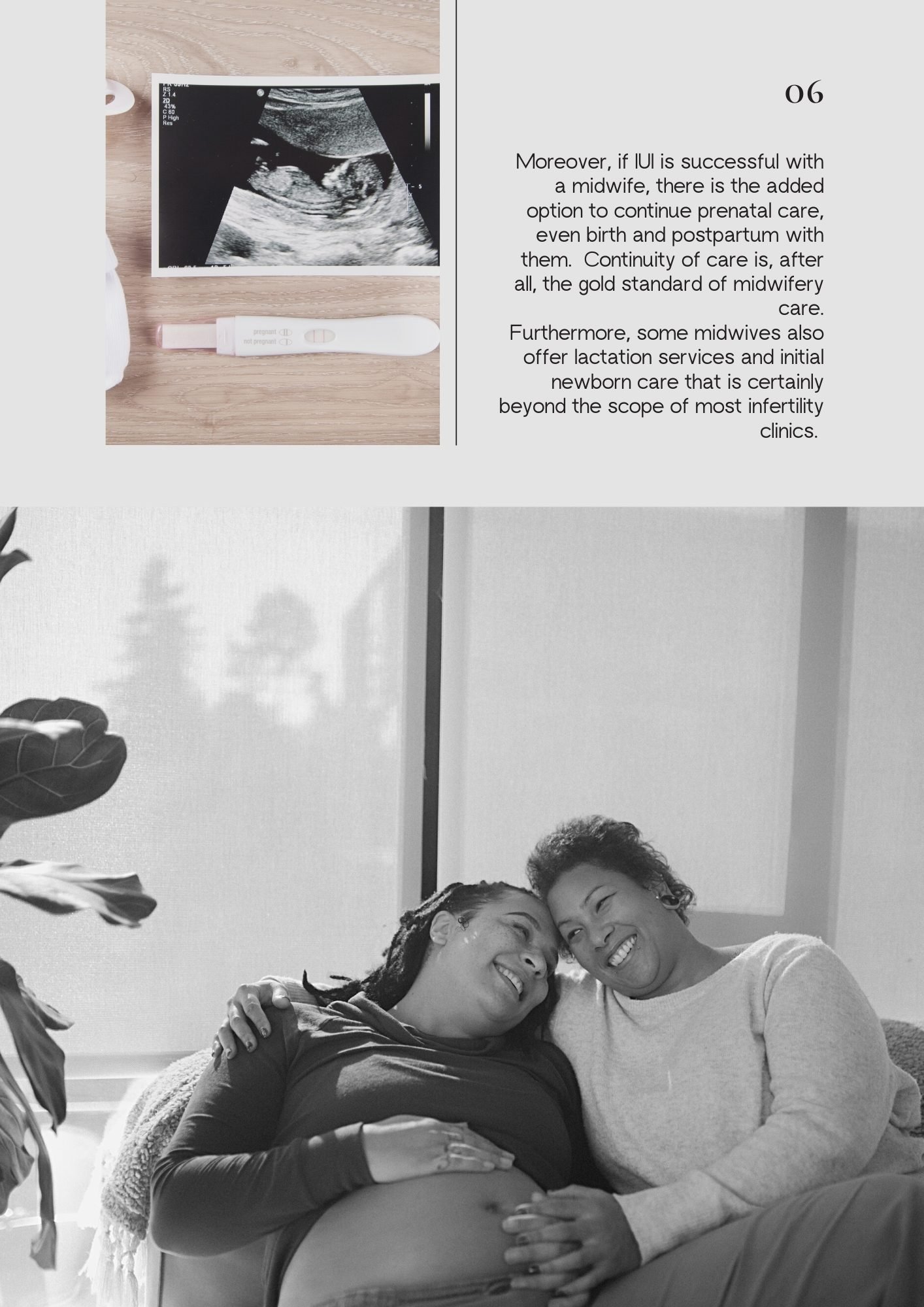
Moreover, if IUI is successful with a midwife, there is the added option to continue prenatal care, even birth and postpartum with them. Continuity of care is, after all, the gold standard of midwifery care. Furthermore, some midwives also offer lactation services and initial newborn care that is certainly beyond the scope of most infertility clinics.
Finding a midwife that offers assisted insemination services may be challenging at first, for a number of reasons. Certain database sites, such as “Out Care” or “Be Her Village” may be helpful places to start, but the greatest hurdle to access is a general lack of awareness or continued misconceptions about how one may access fertility services.
Social media seems to become an increasingly popular way for queer and trans families to share their success stories, challenges, or unfortunate experiences of homophobia, transphobia, or simply a general lack of ignorance among the medical industrial complex.
As more midwives expand their care services to include fertility and donor insemination, the public awareness of these beneficial services will hopefully also grow, transforming the way folx access family-building care that is trauma-informed, LGBTQ+ centered, and inclusive.
(end of article)